It’s here!
Today’s the day that the first Hospice Funerals branch in the UK opens for business.
The people of Taunton have been watching the refurbishment of the former charity shop over the last few weeks, as the grey paint (not dark and forbidding) was applied to the exterior and the shiny new furnishings arrived.
Over the grey frosting on the windows, and below the statement (mysteriously missing the possessive apostrophe) Hospice Funerals Vision, the following legend proudly declares to the world in one long sentence, using the word ‘hospice’ four times and ‘exemplary’ twice just to hammer home the point: ‘To provide all hospice communities the choice and experience of exemplary hospice funeral services that uniquely reflect the dedication, warmth and reputation of the hospice movement – an extension of exemplary hospice care – caring, transparent and personal.’
Phew. Try reading that without drawing breath. Particularly if you’re sitting in traffic alongside the new funeral business and the lights are about to change.
Anyway, on the day of the official opening of St. Margaret’s Hospice Funerals’ first branch, we thought we’d offer those considering copying this trailblazing franchisor and opening their own Hospice Funerals franchise partnership the results of the survey that we have been running for the last month.
Trustees of hospices thinking of following St. Margaret’s’ lead might be particularly interested in the responses to Q4.
In total, 719 people from across the UK responded. This is rather more than the 245 people from an unnamed North of England town where St. Margaret’s and their partners, Memoria Ltd, carried out market research prior to launching – and apparently received an astounding 82% approval of their Hospice Funerals scheme!
Our findings were somewhat different to their results. Although we obviously don’t know exactly what question they asked.
Here are our five simple questions.
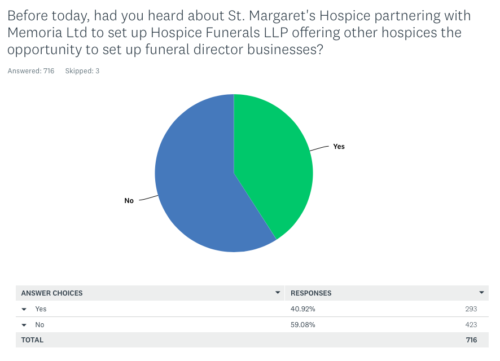
Q1: ‘Before today, had you heard about St. Margaret’s Hospice partnering with Memoria Ltd to set up Hospice Funerals LLP offering other hospices the opportunity to set up funeral director businesses?’
293 people said yes they had.
423 people said no.
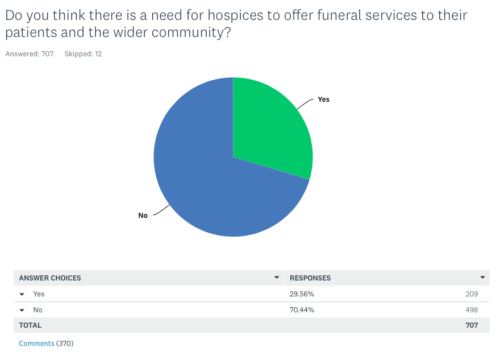
Q2: ‘Do you think there is a need for hospices to offer funeral services to their patients and the wider community?’
209 people said yes.
498 people said no.
(370 people offered their reasons in comments. We’ll add a few of these below to give a flavour of the things said.)
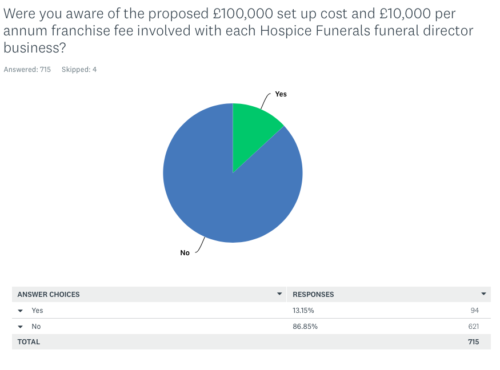
Q3: ‘Were you aware of the proposed £100,000 set up cost and £10,000 per annum franchise fee involved with each Hospice Funerals funeral director business?’
94 people said they were aware.
621 said they weren’t.
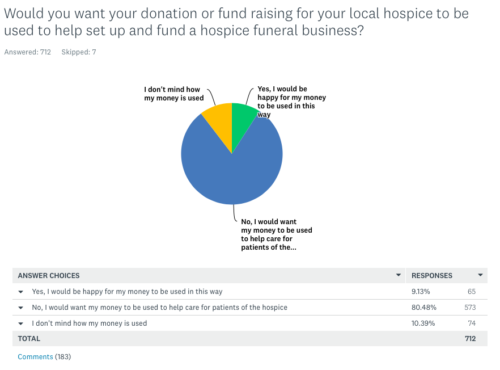
Q4: ‘Would you want your donation or fund-raising for your local hospice to be used to help set up and fund a hospice funeral business?’
65 people said yes
74 people said they wouldn’t mind how their money was used
573 people said no.
(102 people added comment to this question too.)
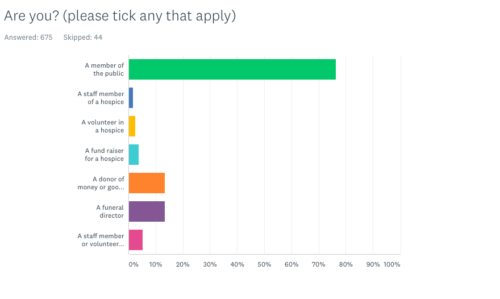
Q5: Are you (please tick all that apply):
A member of the public – 516 people
A staff member of a hospice – 12 people
A volunteer in a hospice – 17 people
A fund raiser for a hospice – 26 people
A donor of money or goods to a hospice – 91 people
A funeral director – 91 people
A staff member or volunteer in another organisation that has links to a hospice – 36 people.
Here are some representative examples of comments in response to Q2. (A complete list of all 370 comments received is available on request.)
“I think this could provide good continuity for families but only if it was done sensitively and not for profit”
“Offering funeral services to patients and the wider community is beyond the scope of health and hospice care, and a potential conflict of interest – i.e. hospice benefits financially from the death of patients. Alternatively, hospices could play a role to support the dying person and their family and carers, and the broader community, with education regarding ceremony and body disposal options, without recommending specific providers; the local community will be better served by each hospice providing information about or links to local, independent, support services and providers.”
“Firstly, I think there are enough Funeral Directors in the UK anyway. Secondly, I feel there is a conflict of interest if the “charity sector” is partnering with a profit making organisation.”
“It should be the patients and their relatives’ decision. At such a difficult time, it would be easy to use the linked funeral provider without it necessarily being the right decision. The whole idea makes me feel very uncomfortable.”
“Ethically the hospice should stand back and let the family chose the funeral director of choice not feel obliged to pay a linked company. All rather distasteful.”
“I feel that families may feel pressured into using these services in gratitude and grief.”
“Their job is to do the right thing on the right side of dying. It’s a conflict of interests to venture into the dead side of dying.”
“There are enough caring independent funeral directors. We don’t need another “big faceless player” on the scene.”
“Hospices provide a different service and conflating that with a funeral service appears to be predatory with grieving families as the victims.”
“There is no need for a linked funeral director, since hospices will all fall within the ‘natural’ catchment areas of a range of existing companies. There could be an argument for resourcing hospice chaplaincy better (Christian and other faiths) so that families are able to have a minister that they already know, and who cared for their loved one spiritually in life, take their funeral.”
“I don’t know a lot about this, but it seems like a helpful service for them to provide.”
“I believe these services should be kept seperate for ethical reasons, the preservation of the notion of hospice care, and for the mental well-being of those in care (I.e. the avoidance of a conveyor belt feeling, as though the living person is perceived as being a resource of value when dead).”
“There is a danger of this option being used by big corporate funeral firms for their own profits while all the time making out they are helping hospices with their funds.”
“I had never considered the idea before, and I suppose it might be the last stop on the continuum of care, but I don’t like the idea. It seems very creepy to have one’s health care team circling like vultures waiting to make money off a funeral.”
“It is a saturated market. There isn’t a need.There should be a demarcation between health and business. The hospice has in essence a captive audience, I honestly think it is an abuse of their privileged position.”
And in response to Q4 – again, a representative sample of the range of comments received from 102 people, with the full list available on request:
“I am happy to help care for patients and to help hospices raise the money needed for their existence. They are an invaluable service. I would not want my money to be helped to support a conglomerate whose directors are set to take funds away from the Hospice.”
“I would NOT be happy to help fund a franchise which would control the business in the style of conventional funeral provision. I would be more than happy to contribute towards a not-for-profit co-operative service provided for & by the community.”
“Simply; because it stinks.”
“I think most people would be shocked to hear that their charitable donations raised in loving memory of relatives they have lost would be used to invest in risky private ventures.”
“I would rather the hospices supported their patients by giving them and their families options to consider. The alternative almost feels like a one stop shop.”
“Hospices need every penny to care for patients and that is why people donate. Using donations to pay for a franchise buy in would be a dishonourable use of funds.”
“I donate to ensure the best care is given at this most difficult time.. The client and family should be able to choose from a range of funeral directors of their choice. I would be very angry and would stop donating if the money was used in any way other than helping people to have the best quality of life until they die.”
“I am assuming that a funeral business would need to make money therefore I would prefer any donations I make would help people at a most difficult time. Perhaps an advice centre within the Hospice would be useful, letting people know what choices are available.”
“This is a ridiculously slanted question. Don’t bother to pretend this is research when it’s clearly a piece of push polling. Unethical.”
Now, we’ve been described as many things in the past, but unethical we ain’t.
We just wanted to know what people actually thought.
Now we’re going to watch and see how this new funeral business with the best branding in town gets on, in an area where bereaved people of the ‘hospice community’ already have a choice of twelve other funeral directors. Many of them are already providing a ‘caring, transparent and personal service’.
We’ll keep you posted.