This post is about psychoactive drugs, so you may want to look away now.
There’s a lot of talk about them just now. Think David Nutt, the man who recently dosed people with MDMA (ecstasy) on television. He thinks ecstasy could be useful in treating depression and (ta-ra!) post-traumatic stress disorder (PTSD). He’s no fool. If a party drug can be used to restore Heroes to health, people are going to sit up and listen.
Good for him. Back in the 1950s psychologists were keen to see whether hallucinogens and other conscious-altering drugs, like recently synthesised LSD, could benefit humankind. Then the hippies hijacked them, they got denounced and outlawed – and research stalled.
Psychoactive drugs are still recovering from disrepute, so much so that it now takes a person with an especially open and enquiring mind to see them for what they are.
Psychoactive drugs can be useful in palliative care. Palliative care recognises the importance of spiritual and emotional needs of patients, but is not good at addressing them. Here’s an example of that from the NHS:
The staff in hospital or hospices or care homes will try to find out what is appropriate for people of different cultures in their final hours … This will allow them to make arrangements for your spiritual or religious adviser to visit, if you feel that this is helpful, and to make sure that your body is treated in the appropriate way after death.
Can do better, must do better. There is much to be said for making dying, in Aldous Huxley’s words, more a spiritual, less a physiological process.
So please let me introduce you to the Multidisciplinary Association for Psychedelic Studies (MAPS) website, where you can consider for yourself what more might be done for the emotional and spiritual needs of the dying.
The following is an example from MAPS of some proper, scientific research conducted by proper, dispassionate scientists. It’s extracted from a much longer article by Stephen Ross, MD, so it’s just a taster.
The sicker patients get, the more they want their physicians to talk to them about spirituality, meaning, and beliefs. The problem is that physicians aren’t educated to have these discussions.
Spiritual distress follows when a sudden crisis leaves a person unable to find sources of hope, love, meaning, value, comfort, or connection.
If you look at the prevalence of psychiatric distress in advanced and terminal cancer patients, it’s incredibly high … very few doctors are trained to deal with it.
[In a recent] study, significant correlations were found between spiritual well-being and decreased hopelessness. All this suggests that we need to come up with psychotherapies and pharmacological modalities that address end-of-life distress by increasing spiritual states.
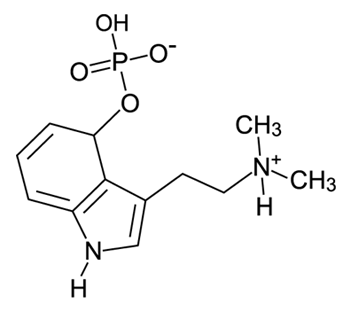
There are 180 species of psilocybin, also known as psychedelic mushrooms … Psychiatric textbooks focus on the negative, frightening, horrible things that can happen under the influence of psychedelic agents … Other facets of mystical states include a transcendence of time and space, a deeply felt positive mood, and a sense of sacredness.
So what happens when someone takes psilocybin? There have been no case reports of human death from psilocybin. We know that it reliably causes mild elevations in blood pressure, but this is not known to be dangerous. Neither is psilocybin addictive. The problem with psilocybin is that people can experience anxiety, fear, panic, and dysphoria.
We have had seven subjects enroll [in a research study]. These subjects are not hippies from the sixties who think it’s groovy to do this again; they are patients who are dying in distress, people in their sixties and seventies facing serious end-of-life phenomena.
The first is a 59-year-old woman. At the end of the session, she said, “I feel light. I don’t know what’s going on, but something has passed from me. I feel so much better.” The next day we asked her how she was doing, and she reported feeling great. When asked about her cancer, she said, “I don’t connect with it anymore.” Two weeks later, two months later, six months later, every single day for her is like Groundhog Day: How are you doing? I feel great. She went back to gardening. She went back to listening to music. She reconnected with meaningful aspects of her life. Although I found it hard to believe at first, I’ve seen it again and again since.
Full article here. MAPS website here. The best way to research the MAPS website is by typing a search term (eg, end-of-life anxiety) into the searchbox top right.

This is very interesting, and not especially surprising. It will be interesting to see where this goes. ‘medicines’, however, no matter how unusual or exotic, will always be a part of the solution, not the full solution. Doctors, and palliative care workers still need to be better trained to deal with the spiritual needs of patients and, indeed, to understand what ‘spiritual needs’ means. For some there will be a big overlap with ‘religion’ and for others there won’t. Serious progress is unlikely to be made until the realisation is made that everyone has ‘spiritual needs’….even atheists. maybe its the… Read more »
Jenny, how good of you once again to contribute so much to the discussion. We really do value your learning and your humanity. What do you think of the definition of spirituality in the Ross article? I like it. And I like this: ‘The behavioral component of our spirituality can be expressed in a variety of ways; for some, it is expressed in an organized religion, while others do so through altruistic, creative, or scientific pursuits. Einstein was Jewish but not religious, for example. He found spiritual connection in the scientific pursuit.’ I agree with you that spiritual needs cannot… Read more »
Oh, I agree with you entirely, but I think we need a variety of approaches of which this, I suspect, is one. I have not read the full article yet (for the very good reason that we are having a half day today to go to a local garden centre’s launch of Christmas decorations (yes, we’re soft!) but I will, and I’ll let you know what I think. defining ‘spirituality’ is certainly a thorny issue! As for pain as a way to enter different states of consciousness…absolutely! (don’t know about mescalin in particular but I may be wrong 🙂 )… Read more »
There was of course the Marsh Chapel Experiment, also known as the Good Friday Experiment in 1962, initiated by Timothy Leary and conducted with divinity students at Harvard. Two groups were either given a placebo or psilocybin, and almost everyone who took the psilocybin had a profound religious experience. For me, these drugs are simply a different medicine. If you are in severe pain, you are given morphine. If you are in spiritual pain, you should be able to take MDMA. On the MAPS, site there is an incredible account from a mother who overcame her previous disapproval of illegal… Read more »
I have now read the full article, and I have to say it is both interesting and extremely well written (except, perhaps, the reference to a ‘Buddhist God’!). I very much like Ross’s definitition of spirituality…although its a bit long for those who want a soundbite! Its not an easy concept to cram into a short definition though! I like the different aspects he mentions, cognitive, behavioural, emotional. Excellent! A lot has been written recently about the physiology and neuroscience of religious expeience. If drugs can induce ‘spirituality’ or ‘religious experience’ and if such things can be documented in terms… Read more »
That, Jenny, wins fact of the week hands down. I totally agree. One does not invalidate the other.